Vimal age 8, was about to have an MRI scan and the doctor told him that it would make a sound, Sunil, his father, was standing outside, but when the process started, Vimal began crying because of the sound.
It is alarming for some and distracting for others, but it does help to get a better and clearer image and understanding of the presumed diagnosis.
There is more to know about MRI scans than that and also why the sound is made. In this article, we will learn the same and more.
What is an MRI scan?
MRI, or Magnetic Resonance Imaging, is a type of imaging that uses a magnetic field and computer-generated radio waves to create a detailed image of your organs and tissues.
According to Wikipedia, “Magnetic resonance imaging (MRI) is a medical imaging technique used in radiology to form pictures of the anatomy and the physiological processes of the body. MRI scanners use strong magnetic fields, magnetic field gradients, and radio waves to generate images of the organs in the body.”

The emergence of imaging technology started with x-ray in 1895, then came sonography in the 1950s, and x-ray further morphed into CT scan in the late 1960s (1967), and then came MRI in the late 1970s (1977). In 1971, Paul Lauterbur at Stony Brook University applied magnetic field gradients in all three dimensions and back-projection methods to create images. He published his work in 1973 in the Nature journal, and in 1974 he published the thoracic cavity of a mouse. In the 1970s, physicists, Peter Mansfield and Paul Lauterbur invented MRI-related techniques, and they were conferred with the Nobel Prize for Medicine or Physiology.
How is an MRI scan done?
The human body is mostly made up of water molecules, which are made up of hydrogen and oxygen atoms. Each hydrogen atom includes a proton, a much smaller particle. Protons are tiny magnets with a high sensitivity to magnetic fields. When you lie down in front of the intense scanning magnets, the protons in your body align in the same direction that a magnet could pull a compass needle.
Short bursts of radio waves are then sent to certain regions of the body, misaligning the protons. When the radio waves are switched off, the realignment of protons happens. This produces radio waves, which are picked up by receivers. These signals pinpoint the exact location of the protons in the body. They also help identify between different types of tissue in the body, since protons in different types of tissue realign at different rates and provide distinct signals.
Signals from millions of protons in the body are combined to form a detailed image of the inside of the body, similar to how millions of pixels on a computer screen may produce complex visuals.
Some find it uncomfortable and some feel claustrophobic inside the machine, but an MRI scan is painless and one of the safest procedures. But as it involves magnetic fields, people having a pacemaker, artificial joints, any metal implants, or someone with a tattoo where metallic ink is used, is not recommended.
When patients come for an MRI scan, they are made to lie on a flatbed which moves into the scanner. Depending upon which part needs to be scanned, you will be made to lie on the bed and move inside the scanner head first or feet first. A trained radiographer who will be operating the MRI scanner will take images using the computer.
Both of you can talk to each other via intercom, and he can see you all the time. You will be provided with earplugs or headphones due to the noise the machine will be making. The whole process will be over in 30 minutes to 90 minutes.
The doctor would suggest what you should not do before an MRI, which may include not drinking or eating, removing all metallic objects from your body, limiting going to the bathroom, and also telling the technician or doctor if you have any kind of medical condition.
Why is an MRI scan done?
Various tests are performed to rule out the possibility. One of those tests is also an MRI scan. An MRI is sometimes performed to confirm that the treatment is working as it should. This is the reason an MRI scan is done:
1 MRI scan of the brain and spine to diagnose conditions like aneurysms or blood vessel damage, brain injury, cancer, multiple sclerosis, stroke, spinal cord injuries, and eye and ear problems.
2 MRI scans of the heart and blood vessels were performed to diagnose heart disease and damage caused due to heart attacks, broken blood vessels, inflammation of the tissues surrounding the heart, problems with the aorta, and problems with the structure of the heart.
3 MRI scans of bones and joints were performed to diagnose cancer, arthritis, bone infections, disc problems in the spine, and damage in joints, neck, or lower back pain problems.
4 MRI scans of the breast were conducted to check for the possibility of cancer or re-emergence of cancer after surgery or chemotherapy. A scan is ordered to check whether the implants have not ruptured.
5 MRI scans of internal organs like liver, kidney, ovaries, prostate, and pancreas are ordered as per the doctors’ prognosis, mainly to confirm cancer or that they have seen symptoms of other diseases and to get confirmation, an MRI scan is ordered.
What are the different types of MRI scans?
Functional Magnetic Resonance Imaging
It is also called Functional MRI or fMRI which detects changes and measures the brain activity related to blow flow. This method is based on the assumption that cerebral blood flow and neuronal activity are inexorably related. When a section of the brain is used, blood flow to that section of the brain increases.
The simplest form of fMRI employs the blood-oxygen-level-dependent (BOLD) contrast. This is a type of focused brain and body scan used to map neural activity in humans or other animals’ brains or spinal cords by measuring changes in blood flow (hemodynamic response) produced by brain cell energy utilization.
In addition to identifying BOLD responses from activity caused by tasks or stimuli, fMRI can measure resting state or negative-task state, which reflects the individuals’ baseline BOLD variance.
The other ways of getting the contrast are arterial spin labeling and diffusion MRI. Arterial spin labeling (ASL), also called arterial spin tagging, is a magnetic resonance imaging technique that labels blood as it circulates through the brain to assess cerebral blood perfusion.
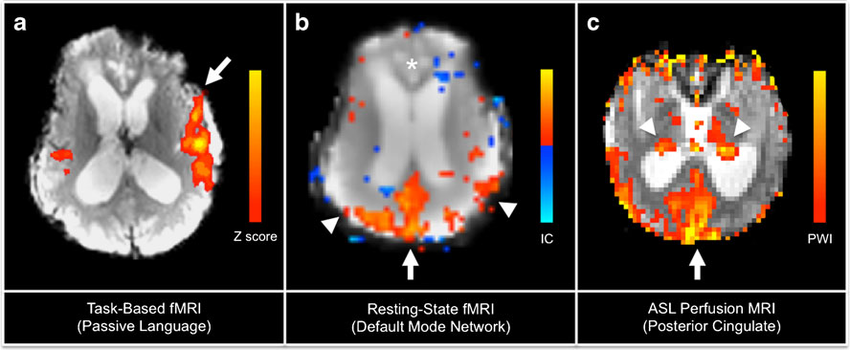
ASL, which was the first of its kind in perfusion imaging, refers to the magnetic tagging of arterial blood beneath the imaging slab without the use of gadolinium contrast. Flow alternating inversion recovery (FAIR) is the most basic ASL method, including two acquisitions of identical parameters except for out-of-slice saturation; the difference between the two images is allegedly purely from inflowing spins and may be referred to as a ‘perfusion map.’
Diffusion-weighted magnetic resonance imaging (DWI or DW-MRI) employs certain MRI sequences and software that generates images from the collected data to generate contrast in MR images through the diffusion of water molecules. It permits non-invasive in vivo mapping of the diffusion of chemicals, notably water, in biological tissues.
In tissues, molecular diffusion is not random, but rather the consequence of interactions with various obstacles such as macromolecules, fibers, and membranes. Water molecule diffusion patterns can thus give detailed information on tissue architecture, whether normal or ill. DWI has been widely used to map white matter tractography in the brain, particularly with diffusion tensor imaging (DTI).
Cardiac MRI
As the name suggests, cardiac MRI is an MRI of the heart. A heart MRI is a scan of your heart that employs radio waves and magnets to create images without allowing anything visible or palpable into your body. A cardiac MRI may show the various components of your heart (such as chambers, valves, and muscles) and how well they work, as well as how your blood flows. These exact, high-quality two- or three-dimensional images help your healthcare expert figure out what’s wrong and provide a diagnosis.
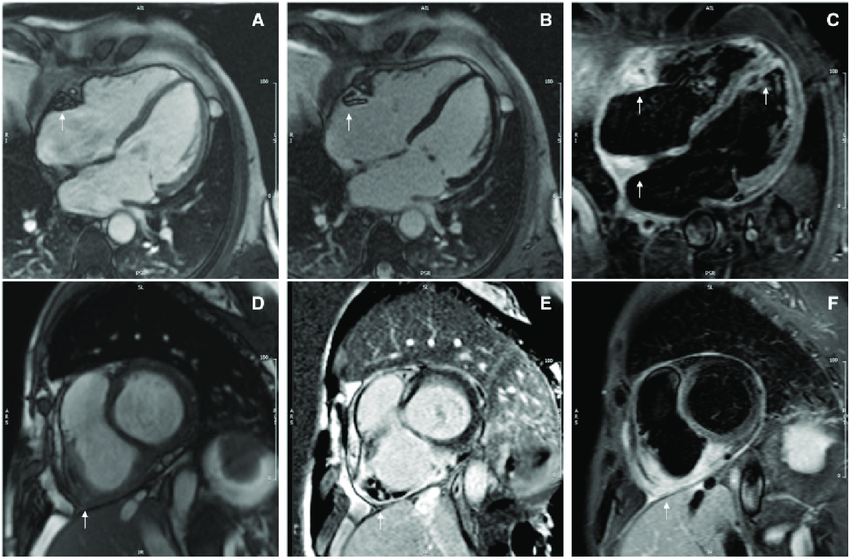
An MRI of the heart is performed to diagnose heart disease and damage caused by heart attacks, broken blood vessels, inflammation of the tissues surrounding the heart, problems with the aorta, and problems with the structure of the heart.
Breast MRI
Breast magnetic resonance imaging (MRI), often known as breast MRI, is a technique used to detect breast cancer and other abnormalities. A breast MRI produces a series of pictures of your breast. Breast MRI scans are combined with a computer to produce detailed pictures. Following a cancer-positive biopsy, a breast MRI is commonly performed.

A breast MRI can reveal to your doctor the severity of your condition. Breast MRI might be used in concert with mammography as a screening approach to detect breast cancer in some people. Women who are at high risk of breast cancer, have a strong family history of breast cancer or have a hereditary gene mutation.
Magnetic Resonance Venography
A diagnostic process that produces comprehensive pictures of organs and structures within the body using a huge magnet, radio frequencies, and a computer. An MRV visualizes the veins using magnetic resonance technology and intravenous (IV) contrast dye. The contrast dye makes the blood vessels on the X-ray picture look opaque, allowing the clinician to view the blood vessels being checked. In rare circumstances, MRV can aid in the detection of reasons for leg discomfort other than vein issues.
MRV is used to assess blood flow in veins and identify blood clots and other anomalies. The bulk of serious blood vessel ailments, such as stroke and heart attack, is caused by artery issues rather than vein issues.
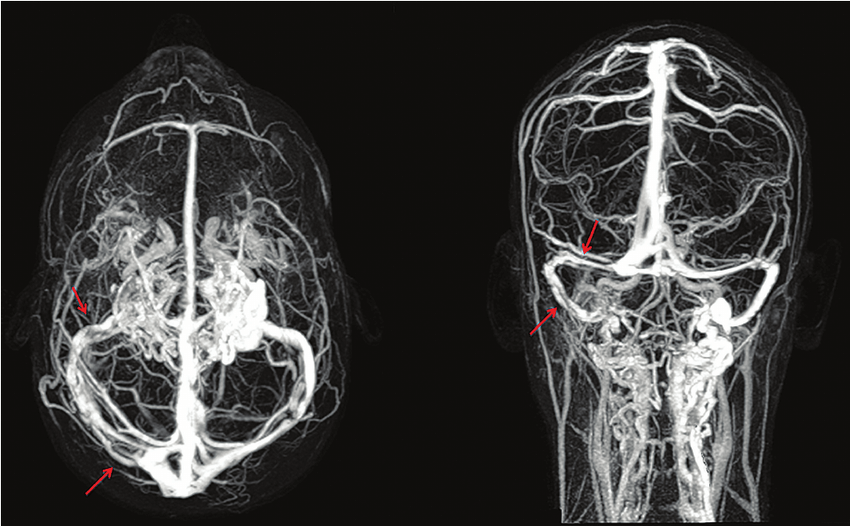
If you need an MRV, your doctor is most likely evaluating you for a less common health issue that may take some time to identify. Structured vein anomalies or blood flow concerns in the brain, developing venous abnormalities in a newborn, and/or blood clots that harm veins rather than arteries are examples of these issues. There is one very specific condition called cerebral venous thrombosis, in which blood clots in the veins of the brain happen.
Non-Contrast Magnetic Resonance Venography
An MRA uses a machine to generate a magnetic field that uses radio wave energy pulses to create real-time images of blood vessels and blood flow throughout the body. MRAs can be performed with or without a contrast medium (medical dye). When used without dye, it is known as a non-contrast MRA.
A non-contrast MRA is safer for patients who cannot handle the contrast dye used to get crisper diagnostic pictures. Newer versions of MRAs may provide highly precise pictures that capture even minute aspects of interior vascular networks without the use of contrast dye. In other words, a non-contrast MRA allows your doctor to inspect small blood arteries.
This enables your physician to identify the atherosclerotic disease (a plaque build-up that can block the flow of blood in your arteries). An MRA is non-invasive, as opposed to standard angiography, which entails inserting a specialised flexible tube (catheter) into the body to generate pictures. MRA is a relatively new breakthrough in the field of MRI (magnetic resonance imaging).
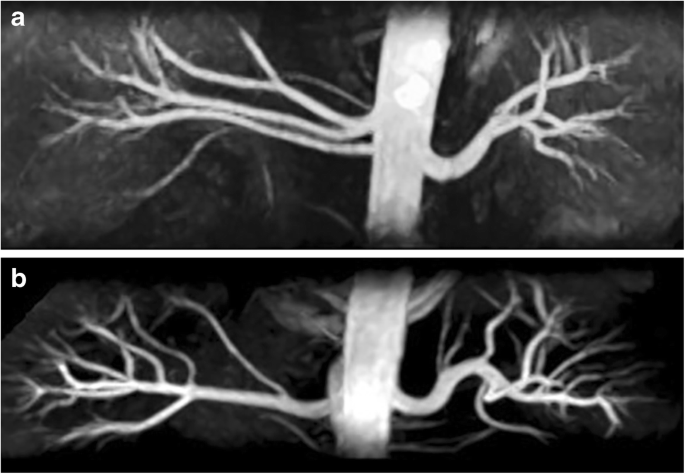
An MRI may view many different regions of the body, including bones and joints, soft tissues, muscles, internal organs, and blood vessels, but an MRA is specially designed to show the arteries and veins. Both technologies have a lot of overlap, and methods for producing non-contrast MRA (NC-MRA) have been around since MRI was invented.
Open High field MRI
Though traditional “closed” MRI scanners have improved and adapted to patient comfort by incorporating wider tables, larger tubes, and other features, people who suffer from real claustrophobia and anxiety issues, suffer even in the presence of these.
For some who are claustrophobic, open MRI machines may be preferred. It is also more comfortable for people who are significantly overweight or obese. The high-field open MRI gives additional space and ventilation for enhanced comfort. The holes in open MRI machines are bigger and less constrained. They allow workers to communicate with and maintain eye contact with the patient at the table, resulting in a more empathetic and peaceful meeting.

Because patients must stay still for shorter periods of time, quicker scanning rates reduce picture contamination caused by patient movement. On the initial try, images are typically crisper and more acceptable.
How to read an MRI report?
A magnetic field, hydrogen ions, and a radio frequency (RF) pulse are used to power MRI machines. When a patient is placed in a high magnetic field, their hydrogen ions align in the direction of the magnetic field. An RF pulse will be used to modify the direction of alignment of these hydrogen ions. When the RF pulse is withdrawn, the ions attempt to re-align with the magnetic field and release a signal. The type of tissue (fat, muscle, or water) in which the hydrogen ion is detected determines the strength of this signal.
Using these concepts, you can configure the machine to identify signals from different magnetization ranges and planes. This is where “weighted imaging” comes into play. We may also instruct the computer to ignore particular signal levels in order to “suppress” them while processing images; these are known as “fat suppression” sequences.
MRI can also be utilised for dynamic imaging. DWI can, for example, investigate the diffusion of water molecules, whereas MR angiographic techniques may investigate the macroscopic flow of blood.
There are some common imaging and sequencing approaches with different combinations of factors. They are as follows-
T1 & T2 weighted images
T1 and T2 pictures show distinct tissues depending on the timing of the RF pulses. The main distinctions between the two are as follows:
T1: one tissue is bright, that is FAT, T1 is the most ‘anatomical’ of the images (Figure 1). The cerebral fluid (CSF), on the other hand, appears bright in T2 due to its high-water content.
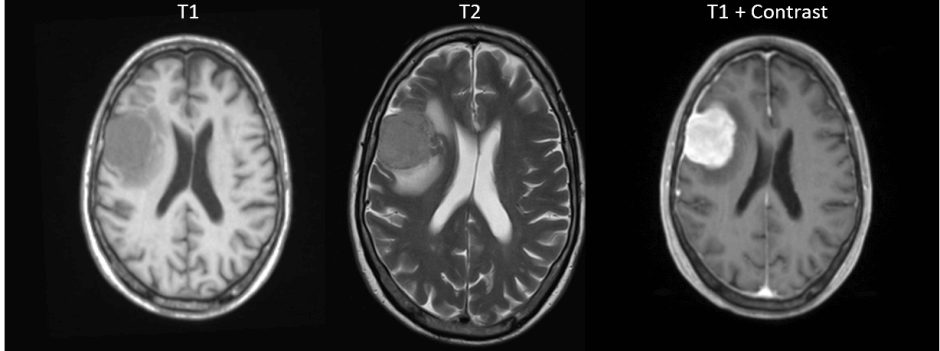
T2: Two tissues that are bright are FAT and WATER (water is white in T2). T2 is the most often utilized. However, T1 can be used as a reference for anatomical structures or to differentiate between fat and water strong signals.
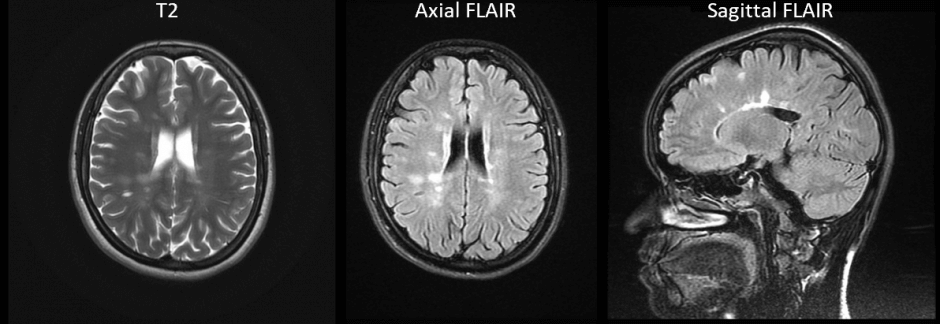
There is an inversion recovery sequence or IR sequence, which is a type of T1 and T2 image where certain tissues are nullified based on their inversion timing and, by doing so, stop the tissues like fat and CSF from appearing as bright singles.
STIR or Short Tau Inversion Recovery is based on the T2 image. Wherein fats and other materials that are similar to singles are eliminated.

FLAIR, or fluid-attenuated inversion recovery, is the same as T2 but here CSF singles are nullified. This comes in handy when you have to study and evaluate structures in the CNS, or central nervous system.
DWI or Diffusion-weighted imaging and Apparent Diffusion Coefficient (ADC)
Diffusion-weighted imaging is an imaging method where the diffusion of water is combined with a T2 image. As DWI is sensitive to water diffusion, ischaemia can be visualized within minutes of occurring, thereby identifying physiological changes that happen just after a stroke. High signals at first, but they get lower after several weeks in early ischaemia.
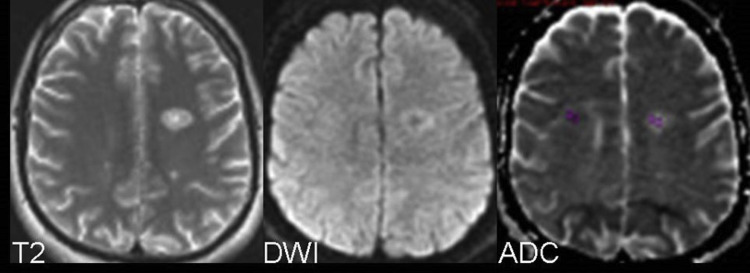
ADC confirms actual limited diffusion in DWI by measuring solely the diffusion of water with no T2 combination. The signal is initially low, but it gradually improves over several weeks and remains high, so it should always be used along with DWI.
What is the side effect of an MRI scan?
An MRI scan is a painless imaging technology that avoids the use of x-ray radiation. An MRI scan has no known negative effects. The advantages of an MRI scan are related to its precision in detecting structural abnormalities in the body.
Patients with metallic objects in their body must notify their doctor or the MRI staff before the treatment. Metallic chips, surgical clips, materials, or foreign material (for example, artificial joints, metallic bone plates, or prosthetic devices) can significantly distort MRI images. Patients who have pacemakers, metal implants, or metal chips or clips in or around their eyes cannot be scanned with an MRI because the magnet may move the metal. Individuals with artificial heart valves, iron ear implants, gunshot fragments, chemotherapy, or insulin pumps should also avoid MRI screening.
During the MRI scan, the subject is enclosed in a compartment within the magnetic tube. Some patients may experience claustrophobia during the procedure. As a result, persons with a history of claustrophobia should notify both the practitioner requesting the test and the radiology professionals. A little sedative may be taken before the MRI scan to help alleviate this discomfort. During the MRI scan, the MRI crew is usually present. Furthermore, if the patient is unable to withstand the scan, there is usually a mechanism for the patient to communicate with the personnel (such as a buzzer carried by the patient) that may be used for contact.
Conclusion
With time, the imaging methods got better, and with MRI coming into the picture, the imaging has been enhanced to an amazing degree. With the advancement of technology, the size of the scanner is becoming smaller and more portable. In the coming years, AI will be part of the software, and the detailed detection and nullifying of either tissues or water will be done in a more efficient way to get to the bottom of a problem. Along with that, the time required to do the scan is also reduced. With the advances, the patient no longer has to lie down; now they can sit, and scans are taken with the machine, which is positioned at 90 degrees.
As open MRI machines are available on the market, the feeling of claustrophobia is also reduced. Along with that, the noise factor has also been reduced now, and MRI scans are now used in surgery to get a better understanding of the condition. Also, with time, you will see the cost of an MRI go down.
MRI, when it came to the foray, was a technological improvement from what was there, and it is still changing and getting better. With time, technology will improve dramatically. The only factor that might be a roadblock to its progress will be the price point. With technological advancement, the price will drop and the technology will be available to all.
FAQ
Can you tell if a tumor is cancerous from an MRI?
Yes, it can tell if it’s cancerous moreover it can also tell if cancer has spread or not.
Does MRI show inflammation?
Yes, it shows inflammation. A doctor can see the inflammation and distinguish it from MRI.
Can MRI cause joint pain?
No, it doesn’t cause joint pain, but if you ling still for 30 minutes to 90 minutes it might cause some discomfort in the leg.


1 thought on “MRI Scan 101: A comprehensive introduction”
Thank you.